Category: General Health
Achieve healthy weight control during pregnancy
As we journey through pregnancy, we want what is best: to grow a healthy baby without compromising our own health. In order to achieve this, our body weight, body mass index (BMI) and health before we become pregnant are important factors, as is the quality of our diet, weight gain during pregnancy, and how active we are.
Pregnancy weight management can be a complex and difficult subject. In any case, gaining or losing too much or too little weight isn’t good for women or babies, as this can affect the pregnancy, delivery, and future health of both. Besides that, what else should you know? Let’s simplify this topic for you, and also explore how you can make small changes in your life that facilitate the process.
Why is gaining too little weight bad for the baby?
- It significantly increases the long-term risk that your child will become overweight/obese in the future.
- The risk of premature birth and low birth weight increases – even if the mom was overweight to start with. Low birth weight is one of the top risk factors for infant illness and death.
Why is gaining too much weight bad?
- For the mother: the risks go up for gestational diabetes, high blood pressure in pregnancy/preeclampsia, and C-section delivery
- For the baby: the risk goes up for stillbirth, premature birth, birth defects, obesity, diabetes, and having a very large foetus (over 4kg)
- The risk is highest among women who are both overweight beforehand and gain excessive weight during pregnancy
What does gestational weight gain consist of?
It comprises the growth of the foetus, placenta, breast tissue, fluids (blood volume and amniotic fluid), and fat accumulation in the mother. The weight increase during pregnancy is necessary for the healthy development of the foetus but should be done gradually. The first 16 weeks of pregnancy should not see much weight gain.
The typically recommended weight gain is as follows, based on your weight when you become pregnant (Adopted from Institute of Medicine Guidelines):
- for underweight women (BMI less than 18.5), it is 12.7-18.1kg;
- for normal-weight women (BMI between 18.5 and 25), it is 11.3-15.9kg;
- for overweight women (BMI between 25 and 29), it is 6.8-11.3kg;
- for obese women (BMI of 30 or greater), the recommended weight gain during pregnancy is 5-9.1kg. For some women, this gain can be entirely accounted for by the normal foetal growth and changes of pregnancy, and obese women may not need to change calorie intake, but focus on improving diet quality. Don’t cut calories unless medically advised.
You can calculate your own BMI here.
Here are the 6 things you should pay attention to:
-
- Ensure you are at a healthy weight before you conceive. If you are overweight, it is good to lose some weight (even just a little) before conceiving. Yes, even though you will gain weight in pregnancy.
- Eat a nutrient-dense diet focusing on real foods. Limit processed foods (refined foods like ‘instant’ foods, snacks like chips, chocolates and cake, ‘white’ grains, fizzy drinks whether ‘diet’ or not, etc.) because they are less nutritious than whole foods.
If you consume calories from real, whole foods, you’ll get more nutritional value: fruits, vegetables, nuts, seeds, eggs, legumes, meat, fish, whole grains, yoghurt and other dairies. Instead of a bag of chips, you could eat an apple with nuts, for example. But sometimes it’s perfectly OK to have the chips or ice cream – in moderation, remember? It’s not about starving yourself, but about eating the right types of food most of the time, for the best positive effect on your wellbeing. See a nutritionist if you need help tailoring a balanced way of eating that works for you.
- Eat a nutrient-dense diet focusing on real foods. Limit processed foods (refined foods like ‘instant’ foods, snacks like chips, chocolates and cake, ‘white’ grains, fizzy drinks whether ‘diet’ or not, etc.) because they are less nutritious than whole foods.
- You don’t need extra calories in the first trimester. Eat as normally and healthily as you can, given that you may feel nauseous and tired at times.
- In the second and third trimesters (months 4 – 9), the general advice is to up your calorie intake by about 340 to 450 calories a day, depending on your activity level. However, this may not apply to you if you were overweight/obese to start with. You don’t have to eat all the ‘extra’ calories in one go, but here is just an idea of what that looks like with real food.
- 300 calories are 100g plain Greek yoghurt + 1 medium banana + 15g almonds
- 350 calories are 2 scrambled eggs + 1 slice of whole-wheat toast (buttered)
- 400 calories are 100g fish + 100g sweet potato + 1.5 cups broccoli with 1 teaspoon dressing + 1 cup strawberries
- 450 calories are 100g chicken in a soy-chilli-sesame sauce + 100g green beans + ½ cup cooked brown rice
- You may need to change the way you eat as the pregnancy progresses. For example, due to pressure on the digestive organs, some women need to eat more often but with smaller portions to feel comfortable. By the way, you will actually need more calories for breastfeeding!
- Stay active.
- Obstetricians, gynaecologists and exercise physiologists advise pregnant women with no contraindications to be active daily throughout their pregnancy. For meaningful health benefits, they recommend at least 150 minutes (2.5 hours) of moderate-intensity physical activity each week (spread over 3+ days per week).
- Many types of exercise are beneficial: aerobic, resistance training, and yoga/stretching.
- If you’ve aren’t active, there are easy, enjoyable and safe ways to start moving your body more, like walking, swimming, dancing. It doesn’t have to feel like ‘a serious workout’ in order to benefit your wellbeing.
- If you already exercise, there are ways to adjust your routines to be safe, effective and enjoyable during pregnancy.
- Check with your doctor that you are cleared to keep exercising, and ensure your trainer is qualified to train prenatal and postnatal women and understands contraindications.
- In the second and third trimesters (months 4 – 9), the general advice is to up your calorie intake by about 340 to 450 calories a day, depending on your activity level. However, this may not apply to you if you were overweight/obese to start with. You don’t have to eat all the ‘extra’ calories in one go, but here is just an idea of what that looks like with real food.
- Ensure you are at a healthy weight before you conceive. If you are overweight, it is good to lose some weight (even just a little) before conceiving. Yes, even though you will gain weight in pregnancy.
As we can see, pregnancy isn’t neither an invitation to “eat for two” calorie-wise nor a time to diet, starve, skimp on nutrients, over-exercise, ‘detox’ or do other things with a fear of weight gain. An optimal balance can be reached with moderation and targeted advice from your healthcare provider, based on your starting point health-wise as well as what comes up during your check-ups.
Weight management during pregnancy may first sound intimidating, but once you get into your momentum, things will feel a lot easier and like every other thing you are motivated to do, you will become proficient at it.
Sources and references:
Healthline – Weight Before Pregnancy Is a Bigger Health Factor Than Weight Gain During Pregnancy
Healthline – Don’t ‘Eat for Two’ While Pregnant
Healthline – Why Some Pregnant Women May Not Need to ‘Eat for Two’ to Stay Healthy
Healthline – Why Pregnant Women Shouldn’t Gain Too Much or Too Little Weight
Health Hub SG – Pregnancy Weight Gain Checklist
Grow by WebMD – Pregnancy Weight Gain Guidelines Explained
Grow by WebMD – The Importance of a Healthy Pregnancy Weight
Tips to Stay Healthy While Traveling
With the world opening up more and more post-pandemic, it’s a happy news that international travel is once again available for work or play. Learning how to stay healthy during your upcoming journeys has become more important than ever, not only to make the most of your long-awaited trip but also as we all should, to adapt to the new norm of being more careful after a global health crisis.
Travelling can impose challenges on our health, especially the Long-haul ones. Our immune system takes a knock when our sleep/wake cycles are disrupted (even without jet lag). Blood circulation and lymph flow become sluggish from sitting for long periods, and even feeling stressed before/during a trip can reduce our immune activity, leaving us more prone to getting sick.
Take a look at our handy checklist of things to help you to organize your thoughts, give you peace of mind and keep your immunity as strong as possible. The more informed you are, the better – less is never more when it comes to preparing for medical and health matters.
What to prepare before your trip?
Covid is still the main concern for travel, so you might want to check the disease incidence where you are and at your destination, in case this affects your plans. And don’t forget to check the requirements at all locations – we have so many things to organise now, like tests and certificates.
(i) Speak with your GP prior to travel. Your doctor can help you with:
- new/repeat prescriptions (especially if you have a chronic condition)
- advise you on over-the-counter medications to carry with you, and
- help you with pre-trip vaccinations or tests. You may be due for booster shots (e.g. influenza, hepatitis, Covid-19) or you may need to get a different jab that is specific to your destination. Start the process early, so that the protection from immunisation is already effective by the time you start your trip.
(ii) Pack a medicine kit and your medical information. Put this in your cabin baggage because checked baggage can be delayed/lost. This can include:
- prescription medications, especially for those who take insulin, blood thinners, antidepressants, etc.
- over-the-counter medications (antihistamines, painkillers, oral rehydration salts, anti-nausea/diarrhoea drugs) and other items (contraceptives, probiotics, etc.)
- a thermometer, and an oximeter if you have one
- Covid rapid tests
- first-aid items (plasters, antiseptic cream)
- medical records that could be helpful if you see a doctor at your destination. For example, if you need regular monitoring or you have a history of surgeries
- your doctor’s contact details
- your medical (and other) insurance policy documents
- original packaging: this is the safest way to carry medications; you may also need to prove that they were prescribed to you by a doctor, so do check
(iii) Pack a basic care kit for the plane, i.e. things that keep you comfortable, warm, hydrated and relaxed. A good selection would be:
- hand sanitiser, several masks, nasal spray (saline or decongestant), mouthwash/gargle, moisturiser, lip balm, eye drops, ear plugs, healthy snacks, water, and whatever helps you relax and sleep (herbal teabags, an eye mask, a travel pillow, a large scarf/clothes that layer)
Travelling when sick (even when the illness is minor) can spread disease, and it can make your experience very unpleasant. If you have any symptoms of illness, please contact your airline about rescheduling your flight.
Things to pay attention to during your trip
- Get up and move around, stretch or move your body on the plane. If you have to transfer, don’t spend the layover just sitting, walking or moving as much as you can. Being sedentary can bring on muscle or joint pain, and increases the risk of potentially dangerous blood clots.
- Stay hydrated at all times – drink enough water and electrolytes, and minimise alcohol and caffeine.
- If you’re going across time zones, aim to eat and sleep at the right times in the destination time zone. Get early morning sunlight in your eyes to help your body clock reset.
- Take your medications as directed and on schedule.
Coronavirus is still around us
The newer Covid-19 variants tend to be more transmissible than the earlier types, so we can still catch and spread this illness even if we are fully vaccinated, but the jab does protect people from the worst effects.
Stay mindful of what you already know about how to reduce your risk of catching Covid-19 (and this applies to many other infectious diseases):
- maintain physical distancing
- wear masks properly
- practise good hygiene (wash your hands properly and frequently, and avoid touching your face). Soap and water are preferable, but of course, sanitiser is useful because it’s portable.
- vaccinate to protect yourself and reduce your risk of severe disease, ask your doctor to check your medical history (such as prior vaccination/Covid-19 infection or contraindications) to see if you are due a vaccination/booster.
The situations with a higher risk for contracting Covid-19 include close contact, crowds, and enclosed spaces (poor ventilation) for prolonged periods – just like planes, trains and other modes of transport. Infections that spread on planes happen most often when people are within 2 rows or 2 metres of a Covid-19 infected person (remember this when lining up). People can be infectious before they realise they are ill, that’s why measures to minimise the spread are so important.
While travelling, some airlines/airports/countries now specify which types of masks are necessary (if any), so do check and ensure you have enough masks of the correct type. Of course, you can still wear masks in places that no longer require them. The nice thing masks also help to moisten the air in and around your nose, so it is less drying on a flight.
What about Monkeypox?
Your overall risk of getting monkeypox is low, so don’t panic! Monkeypox is a viral disease originating in animals. It spreads through skin/membrane contact with the body fluids of infected people/animals, or via contaminated objects. The good news is it is not airborne, so it is much harder to catch than the coronavirus. Common symptoms include fever and painful blisters or a rash.
Some of the measures we already follow to reduce Covid will also reduce your risk of contracting monkeypox. In other words, basic hygiene, such as frequent hand-washing, covering wounds, not sharing utensils/glasses, and practising safe sex.
Last but not least, we must emphasize that even if you are really busy with all the activities and appointments planned during the trip, be sure to take care of yourself before, during, and after. Staying healthy with a balanced lifestyle and diet means your immune system will be at its best, and prevention is better than cure. This means getting enough rest at the right times, exercise, food, water, sunlight, and supplements if needed.
Bon voyage!
Source and References
Healthline – U.S. Officials Will Release Nearly 300,000 Monkeypox Vaccine Doses to Fight Outbreak
Healthline – How Long Is the Coronavirus Infectious When It’s in the Air?
EverydayHealth – Holiday Travel in COVID-19 Times: 10 Safety Tips
EverydayHealth – COVID-19 Testing for Travel: If, When, Where, and How
Public Health – Where We Are in the Pandemic
WebMD – Holiday Travel Advisory
Medical News Today – What to know about flying during the COVID-19 pandemic
Physical Signs That Our Hormones Are Out of Balance
Understanding our hormones is just about as complicated as trying to learn a new language. We know they exist, and that they are important, but we don’t fully understand what our bodies are trying to communicate to us. Hormones play an instrumental role in how our bodies function. They are the chemical messengers that travel through our bodies to drive function in our metabolism and reproduction. When our hormones are imbalanced, they can have some major side effects that should not be glossed over.
Skin
There are various physical signs that our body sends to us when our hormones are imbalanced. The first and most noticeable sign is our skin, which includes dry skin, rounded face, darkening skin, especially along the neck, and groin, and acne on the face, chest, or upper back. A shift in hormones can leave our skin dehydrated, which causes dry patches. Commonly seen during and after menopause, the drop in oestrogen and progesterone, the reproductive hormones, can lead to collagen depletion in our skin and results in a loss of skin elasticity and firmness, which then women feel drier and appear more wrinkled.
Out of all the skin issues, acne could be the most bothering. There are hormone receptors on our skin, and abnormal levels of those can overstimulate the glands and secrete something called sebum, which then leads to the formation of acne.
Hair
The next sign is excessive hair growth or hair loss. Most women have some hair throughout their body, but if it starts becoming excessive in abnormal areas, like the face, then it can be hormone-related. When hormones like testosterone drop in the body, they have a bigger impact on the physical symptoms, like hair growth.
On the other hand, when the levels of oestrogen and progesterone drop after giving birth or during menopause, hair grows more slowly and therefore becomes much thinner. A decrease in these hormones also triggers an increase in the production of androgens that can shrink hair follicles, resulting in hair loss on the head.
Menstruation
Severe PMS and irregular periods are very common signs. Normal cycles are supposed to occur within 21-35 days, so if it is consistently absent or occurs outside these days, it’s likely that our progesterone and oestrogen are too high or too low. Vaginal dryness does happen from time to time to every female, but if it happens too often, then quite possibly, our oestrogen level is dropping, which reduces vaginal fluids.
Weight
Sudden weight changes can also signal hormonal issues. There are hormone receptors in fat cells and oestrogen affects the metabolism. When we’re feeling a little more down than normal, irritable, or overly sensitive, this may be due to fluctuating oestrogen which can then impact the levels of leptin, the hunger-driving hormone. This, in turn, can affect our eating habits and lead to an increase or decrease in weight.
Our thyroid is largely connected to hormone levels. Our thyroid impacts how our body metabolizes food. This can cause weight loss if there are too many hormones in our bodies. On contrary, in hypothyroidism, which stands for inactive thyroid or low levels of thyroid hormones, our body’s natural functions slow down. This could make it more difficult to lose extra pounds and maintain a healthy body weight.
Although oestrogen levels can be low in women for various reasons, the most common reason for that is menopause. When oestrogen level drops during menopause, estradiol, the major oestrogen hormone that regulates metabolism and body weight also drops, and what is next? Many women would experience weight gain around their mid-section and abdomen during this time in their life. Those are fat built up in the belly and around the organs that can cause many potential health issues such as type 2 diabetes, and heart disease.
Hot flashes and headaches
Hot flashes are sensations of heat, sweating, flushing, anxiety, and chills that last from one to five minutes. This is a known menopause symptom due to declining oestrogen levels. Then we have headaches, which come with the drop in oestrogen and strike right before or during our period. If they surface each month, then that is a sign it was due to shifting hormones.
Everything within our body is connected. Each and every part that resides within us plays a pivotal role in how we function. Hormonal imbalances are like a weak link in a chain. If one link is off, the strength dissipates. Blood and saliva tests can be done to measure hormone levels. If any of the above symptoms are something you are experiencing on a regular basis, we recommend getting them tested to have peace of mind, and you and your doctor can work together to get your body back on track. Hormonal balance isn’t something to overlook, as down the line it can become greater health issues.
Sources and references:
Healthline – Everything You Should Know About Hormonal Imbalance
Healthline – Everything You Need to Know About Hypothyroidism
Healthline – Menopause Hair Loss Prevention
WebMD – Do You Have a Hormone Imbalance?
Medicine Net – What Are the Causes and Symptoms of Hormonal Imbalances in Women?
Medical News Today – What to know about hormonal imbalances
Medical News Today – Can estrogen levels affect weight gain?
Northwell Health – 11 unexpected signs of hormonal imbalance
Women’s Health
10 Health Screenings Every Woman Should Have, Especially If You’re Over 25
Our Health is not to be taken for granted in our modern society laden with stress and sometimes irrational indulgences. Each of us should make time for healthy habits such as exercising regularly and having a balanced diet. On top of those, routine health screenings should also be a part of your health protection measure.
The following 10 health screenings for women are important for females and play a vital role in early detection of various diseases.
Such screenings should be done even if you do not experience existing discomfort, and could make a world of difference in preserving your health and quality of life.
Blood Pressure & Heart Health Screening
Why you need it: To ensure that you are not at risk for heart disease, a leading cause of deaths of women in Singapore. Every day, 17 people die from cardiovascular disease (heart diseases and stroke) in Singapore. Cardiovascular disease accounted for 30.1% of all deaths in 2017. This means that 1 out of 3 deaths in Singapore, is due to heart diseases or stroke.
When and how often: Starting at age 20, you should have your blood pressure checked once every two years. If you have existing conditions such as diabetes, kidney problems and obesity, or a family history of hypertension and heart disease, you may be recommended to have your blood pressure checked at least once a year.
What to expect: During your screening, your doctor checks your blood pressure. Ideally, your blood pressure should be below 120/80 millimeters of mercury (mm Hg) accodring to the American Heart Association (AHA). If your reading is higher than 130/90, you could be developing hypertension.
Your doctor also listens to your heartbeat for irregularities or murmurs, which may indicate medication or further checks. You should also let the doctor know if you have been experiencing chest pains or shortness of breath.
Lipid Profile/ Cholesterol Screening
Why you need it: One of the most effective tools to asses your risk for developing heart disease or stroke is to measure your cholesterol levels. Elevated cholesterol has also been linked to gallbladder disease.
When and how often: If you’re age 20 or older, you should have your cholesterol measured at least once every five years. More frequent monitoring may only be necessary if you have certain risk factors such as diabetes, heart diseases, kidney problems, or have sudden changes in lifestyle causing weight gain.
What to expect: A comprehensive lipoprotein profile measures the total cholesterol in your blood, which includes “bad” LDL (low-density lipoprotein) cholesterol, “good” HDL (high-density lipoprotein) cholesterol, and triglycerides. If you’re at risk for heart disease, some doctors may test your apoB levels, a measure of fat particles in the blood.
Ideally, your total cholesterol levels should be less than 200 milligrams per deciliter (mg/dl); a borderline high reading is between 200 and 239 mg/dl.
Pap Smear
Why you need it: It is the best tool to detect cervical cancer in time for effective treatment. According to the Singapore Cancer Society, cervical cancer is currently the tenth most common cancer amongst women in Singapore. Every year, almost 200 new cases are diagnosed and 70 deaths occur from cervical cancer alone.
When and how often: An initial screening should be performed at age 21 or once a woman is sexually active, up till age 65. Pap smears could be done every 3 years. If you have multiple sexual partners, are a smoker, are HIV positive or have a Sexually Transmitted Disease, you should have a Pap smear screening annually.
What to expect: During the Pap smear, your doctor uses a speculum to widen the vaginal canal. This exposes the cervix allowing a sample of cells to be taken with a small brush. The sample is smeared onto a glass slide and then sent for analysis. The doctor will also perform a pelvic examination to check your uterus, ovaries and fallopian tubes.
Your pap smear results will reflect your reading as normal or abnormal and requiring follow up with the doctor.
Mammogram & Clinical Breast Exam
Why you need it: Mammograms can detect the presence of cancerous lumps even before they can be felt with hand, it is currently the most reliable tool for early breast cancer detection. Despite being the most commonly occurring cancer amongst women in Singapore, more than 90% of women diagnosed with breast cancer at the earliest stage remain well and disease-free after 5 years or more, compared to around 15% for women diagnosed at the most advanced stage.
Different Types of COVID-19 Tests
The differences – COVID-19 Polymerase Chain Reaction (PCR), Serology Antibody and Rapid Antigen Test
What is COVID-19
According to World Health Organisation, COVID-19 is an infectious disease caused by a newly discovered coronavirus. Most infected people will experience mild to moderate illness without requiring hospitalisation.
Symptoms of COVID-19
COVID-19 started off with having fever, dry cough and tiredness as the most experienced symptoms. Once the patients come to the clinic presenting these symptoms, they will be swabbed. However, there seems to be more patients presenting other symptoms:
- Aches & pain
- Diarrhoea
- Sore throat
- Headache
- Loss of taste or smell
- Skin rash
- Conjunctivitis
- Runny nose or nasal congestion
For serious cases, the patient will experience difficulty in breathing or shortness of breath. He or she is likely to have chest pain or pressure and will require hospitalisation.
Of course, there always lies the possible risk of asymptomatic patients who may still be shedding the virus but display no visible symptoms.
What the different types of tests mean
Prices
Preparation before your appointment
To minimise waiting time, we would urge you to complete the online registration form prior to arrival at the clinic.
Please arrive punctually for your test, which will take approximately 15 minutes. You will be ushered to a private room for the test. Rest assured that the room is sanitised thoroughly after each patient’s use.
Test Results
We will send you a sms if your results are normal.
Book An Appointment
An appointment is required before making any trip to the clinic.
To make an appointment, whatsapp / call us at +65 9764 1448 (Orchard).
Fusion Medical@Wheelock
Fusion Medical is registered as a CHAS and Public Health Preparedness Scheme (PHPC) Swab-And-Send Home (SASH) clinic. It is also registered to carry out Predeparture Swabs.
Fusion Medical is able to conduct these tests for children above 6 years old.
Should you have any questions, you may contact us via email.
Pregnancy Myths to be Aware of
Myth 1: Pregnant women need to eat twice as much.
Absolute myth. Don’t do it. You really actually only need about 300-400 extra calories a day after the first trimester. And that’s assuming that you’re starting pregnancy at a normal weight.
Overeating can be harmful to both the woman and the fetus, especially if the diet contains a lot of empty calories.
Women should aim for a gradual increase in calories throughout the pregnancy:
- First trimester: No extra calories are necessary.
- Second trimester: Experts recommend an additional 340 calories per day.
- Third trimester: An additional 400-450 calories per day is the recommendation.
Women should generally focus on continuing with their regular diet, but they should ensure that they are eating nutrient-rich foods.
Myth 2: It’s OK to drink a glass of wine when you’re pregnant.
Unfortunately, there is no safe amount of alcohol nor a safe time in pregnancy when we can be sure that alcohol won’t affect a developing fetus.
A 2007 meta-analysis confirmed that low to moderate alcohol consumption during pregnancy is not associated with adverse neonatal or child outcomes. However, as a result of possible methodologic flaws in these studies, it cannot be concluded for certain that alcohol consumption at this level during pregnancy is safe. Therefore, all major health organizations recommend abstaining completely from alcohol during pregnancy.
Also, I think it’s important to add that it is not safe to drink while you’re breastfeeding, either, because the alcohol does get into breast milk. We don’t know what the safe amount is, and that safe amount may actually change for different women.
Myth 3: Cocoa butter prevents stretch marks.
“Cocoa butter prevents stretch marks.” This is a myth. While cocoa butter is something that many patients like to use, we don’t have any evidence that cocoa butter or anything else that we can recommend will prevent stretch marks.
It’s probably genetic, and, essentially, if you gain too much weight in one spot, i.e. your pregnancy gets really big, you’re more likely to get stretch marks, unfortunately. Therefore, investing into a very expensive cream would not be very useful if you have significant amount of weight gain or you are genetically predisposed to stretch marks.
Myth 4: You can give a cold to your developing baby.
“You can give a cold to your developing baby.” This is a complete myth. Your baby is not going get the cold. Although your baby can get sick if you get something like the flu, which is why it is advisable for pregnant women to have influenza vaccination to prevent your baby from getting really sick. There are some illnesses you can transfer to your baby, but probably not a cold. It is important not to confuse a common cold and influenza (the flu) the flu confused, because “the flu “can make you really sick in pregnancy.
Myth 5: Pregnant women shouldn’t drink coffee.
This is a myth. You can drink coffee. This is one where moderation is the most important thing. In the first trimester, having excessive amounts of coffee have been associated with a higher risk of miscarriage.
Once that first trimester is over, should you go crazy with the coffee? Probably not.
According to the American obstetrics and Gynaecology association, you can consume below 300mg caffeine a day, which is equivalent to : Low-to-moderate caffeine intake in pregnancy does not appear to be associated with any adverse outcomes.
Pregnant women may have caffeine but should probably limit it to less than 300 mg/d (a typical 8-ounce cup of brewed coffee has approximately 130 mg of caffeine. An 8-ounce cup of tea or 12-ounce soda has approximately 50 mg of caffeine), but exact amounts vary based on the specific beverage or food.
Myth 6: Pregnant women shouldn’t eat smoked salmon.
This a myth. You can eat smoked salmon if you like it.
There are a lot of concerns around fish consumption in pregnancy, which is a huge topic. And I talk to my patients about the risk of various types of fish. Women should try to consume two to three servings per week of fish high in docosahexaenoic acid and omega-3 long-chain polyunsaturated fatty acids and low in mercury. These fish include anchovies, Atlantic herring, Atlantic mackerel, mussels, oysters, farmed and wild salmon, sardines, snapper, and trout. Other fish or seafood that have low mercury are safe, but might not provide high amounts of docosahexaenoic acid. These include shrimp, pollock, tilapia, cod, and catfish. Women should avoid fish with high mercury content, including king mackerel, shark, swordfish, marlin, and tilefish. The mercury content of commercial fish can be found here.
Regarding Raw and undercook fish/sushi–Most health organizations advise women to avoid raw and undercooked fish during pregnancy. The concern is the result of the risk of foodborne illness such as bacteria or parasites. However, the fish that typically make up sushi (tuna, salmon, yellow tail, snapper, flounder) rarely carry parasites aside from possibly Anisakis or Diphyllobothrium latum (fish tapeworm), which are uncommon in developed countries and are also not particularly dangerous. Therefore, the risk of infection from sushi in developed countries is likely not significant.
Myth 7: Pregnant women shouldn’t pet cats.
This is a myth. It would be terrible if all pregnant women in the world couldn’t pet their pets, their cats!
There is a concern with pregnant women caring for cats in terms of the litter box, and really the risk is toxoplasmosis. And the risk of exposure isn’t with interacting with your cat, but with changing a dirty litter box. It is actually fairly rare in Singapore for pregnant women to come into contact with toxoplasmosis by coming in contact with cat litter.
Cat feces can carry toxoplasmosis, a potentially harmful disease. As a precaution, therefore, a pregnant woman should either wear gloves to change the litter, wash their hands thoroughly after clearing the cat litter or have someone else do it.
Women do not need to avoid cats during pregnancy as long as they follow this precaution.
Myth 8: Pregnant women shouldn’t fly.
This is a myth. Having said this, there are a few things to think about when flying. I think one of the major issues is that pregnant women are at increased risk for getting a blood clot either in their leg or their lung. When you fly, the air is dry. You’re also more likely just to be sitting for a prolonged period of time. And that just further increases your risk for getting a blood clot. So, I always tell my patient to ensure she is adequately hydrated. You should wear support hose or at least, like, you know, running tights or something that gives you a little bit of support in your legs. You should get up and walk around every hour or so. Some people worry about the air pressure, which makes no sense because it’s a pressurized cabin and this is not going to cause the amniotic sac to break.
Another big concern is cosmic radiation. Study have shown that this is below the threshold level for fetal concerns. Pregnant women may go through security metal detectors as well. The radiation exposure from the newer backscatter units is 5 microrem, which is 1/600 the amount of cosmic radiation from the flight itself.
However, I always tell my patient to be cautious about the travel destination, pregnant women should be aware of the potential infection exposures (including Zika virus) as well as available medical care at each individual destination. Also, as pregnancy progresses, the risk of several pregnancy complications increases. Therefore, although there is no exact gestational age after which women cannot travel, each pregnant woman must balance the benefit of the trip with the potential risk of a complication at her destination.
Myth 9: Exercise during pregnancy can strangle/harm the baby.
This is a myth.
Exercise is actually strongly recommended during pregnancy. In fact it is important for physicians to talk to patients about maintaining physical activity, maintaining exercise throughout the pregnancy, unless there’s a medical situation that comes up that changes those recommendations.
Having said that, it is prudent for women to avoid exercises with a higher risk of injury such as contact sports, downhill skiing, and horse-riding. Women should try to achieve on average 20–30 minutes of moderate-intensity exercise four to five times per week. Pregnant women do not need to ensure their heart rates remain below a specific threshold. Rather, moderate intensity is best defined as 13–14 on a 20-point scale (or the level at which women can still talk while exercising.)
Myth 10: Sex during pregnancy hurts the baby.
This is a big myth. I always explained the simple anatomy to my patient because I think that where the confusion lies –“ the baby is floating inside a pool of water, a big balloon bag (the amniotic sac). And that balloon bag is surrounded by thick muscle -which is the uterus. So there’s just no way that sex is going to get even near the baby”. Sexual intercourse and orgasm are not associated with an increased risk of pregnancy complications or preterm birth.
However, for women with vaginal bleeding or ruptured membranes, it is unknown whether sexual intercourse increases the risk of bleeding or infection. Although there are no data to support it, most authorities recommend avoiding sexual intercourse after 20 weeks of gestation in the setting of placenta previa.
Myth 11: Dyeing your hair is harmful for the baby.
This is another big myth.
Data on safety for specific chemicals are limited, but for an individual pregnant woman, exposure to hair dye results in minimal systemic absorption, so they are presumed to be safe in pregnancy.
Myth 12: Your hair and skin look better when you’re pregnant.
This is a very common myth. Some women may notice increase in hair growth but your skin most likely will not look better. The high progesterone levels that you get when you’re pregnant to support the pregnancy brings out acne. For some of my patients, the acne outbreak in pregnancy often requires topical or chemical peel treatment. However, it is important to always consult your doctor first prior to any of the ski treatment during pregnancy.
Myth 13: Eating spicy foods will induce labor.
This is a myth. So far, no evidence based study have shown that any particular food or physical activity or drink or supplement that actually can induce labor. There are medications to use to induce labor.
Myth 14: Yoga can induce labour.
This is a myth. There a lot of benefits to potentially doing yoga and participating in pregnancy, but inducing labour isn’t one of them. Certainly, more women are using yoga, which may help with relaxation, stress relief, pelvic floor muscles strengthening etc.
Myth 15: Yoga makes labour smoother.
Overall, exercise probably gives you a better labour in the sense that it is usually more efficient. But yoga itself, not necessarily making it smoother.
Conclusion
Many myths surround pregnancy, some of which involve incorrect information or advice that may be harmful. Ultimately, most recommendations are general guidelines and should be individualized to each specific patient as appropriate.
A woman should talk to a doctor before making any significant dietary, healthcare, or lifestyle changes during pregnancy.
Celebrate Life!
Celebrate Life!
In view of the improving advancement in medical science and treatment, having a cancer diagnosis is no longer a death sentence in today’s world. On top of that, with the help of preventive measures like health screening, early detection of cancers have indeed helped improve survival rates.
More patients are continuing to live quality and meaningful lives after their treatment is over. The combination of different drugs administered during cancer treatment often alters the physical appearance in a negative way which can be very difficult for patients to come to terms with. Feeling good about the way they look plays a vital role in the mindful recovery and rehabilitation in the journey back into normal life.
Aesthetic Treatment for Cancer Patients
As an aesthetic doctor providing this service, I feel the most important quality that I have is that I am a cancer survivor. Having completed both chemotherapy and radiotherapy, I have experienced first hand the challenges that come with it. I fully understand the physical and psychological needs that commonly occur to the skin as well as the importance of providing a “safe” space – safe in terms of the frequently sanitised physical environment which is important for immune compromised patients, and comfortable in a place that patients can feel at ease about their condition.
Why does a Cancer Patient need Aesthetic Treatment
When cancer treatment is given, one’s skin goes through a lot of stress and becomes more sensitive. Inflammation, redness, irritation, acne and dryness are some of the many symptoms that a cancer patient can experience in addition to the devastating hair loss side effect. Meticulous and careful assessment of a patient’s skin before recommendation of any treatment is vital. But it is a fact that our skin often needs to be prepped and optimised in order to react well to future treatments.
The ultimate aim of aesthetic treatment is to rebuild and restore the barrier function of the skin to promote the growth of new healthy skin cells in recovery. Of course, the psychological part of the treatment is to have someone share part of the difficult and long journey ahead with you, to rebuild that confidence that may have been lost in the midst of your cancer treatment.
What’s Unique about our Aesthetic Treatment for Cancer Patients
- Communication with oncologists
In some cases, communicating with our panel of preferred oncologists is necessary to ensure that the treatment provided does not clash with any existing cancer treatment that a patient may be undergoing. The timing of when a person can start aesthetic treatment whilst undergoing oncology treatment is also taken into consideration in our recommendations to our patients. If needed, modifications are made to keep the patient safe and comfortable.
- Dedicated room
We have created a dedicated room paying special attention to cleanliness and hygiene as we know how important it is to remain infection free due to the low immunity status during this critical period, and especially during these COVID-19 times. We use mostly disposable items, and those reusable ones are sterilised after each patient’s use. The surfaces and bed are wiped down after each use and our staff ensures that patients are protected from any cross-infection throughout the treatment.
As this dedicated room is meant to be a place of relaxation and tranquility, we added soothing music as well as specially selected essential oils to calm the senses.
My Personal Experience
My skin journey during my cancer treatment
Reflecting back, I knew that my dry and sensitive skin was going to deteriorate during my cancer treatment and so I made changes to my skincare regime to ensure that my skin was well taken care of. I focused on skin hydration and making sure that I used products that were mild and gentle. One of the first aesthetic treatments that I chose to do after completing my main cancer treatment was actually laser hair removal because I had started growing a lot of unwanted facial hair about two months after completing my chemotherapy!
Treatments that can be carried out during the Cancer treatment
During Treatment
- Unique HydraFacial®️
- HydraFacial®️
At least 2 weeks after Treatment
This part will be categorised based on the skin concerns that would have arose as a result of the treatment:
- Enerpeel Pyruvic Acid Peel
- Fotona
- BLUE LED Light
- HydraFacial®
- Oral antibiotics
- Topical antibiotics and retinoid
Skin Dryness
- HydraFacial®
- Rejuran (PDRN)
- Juvederm VOLITE
- Skin CoE microneedling
Skin Dullness
- Cyspera cream
- FOTONA Starwalker Q switched NDYAG laser
Saggy Skin
Excess Hair
- DPL
- FOTONA laser
Body Aches
- Massage
Intimacy after Cancer Treatment
Celebrate Life!
Looking back, I see the experience I have gone through with cancer as a blessing in disguise. I now live everyday with greater tenacity and joy. I am very lucky to have discovered my condition at an early enough stage and been given a second chance at life which I am so thankful for. Read more about early detection and screening for cancer.
The journey for any cancer patient is a difficult one. I hope to be of service to those who may need some assistance in improving their confidence in their road to recovery. We are not cancer patients. We are cancer survivors.
Lets celebrate life after cancer!
Early Detection and Screening for Breast Cancer
YOUNG AND PLANNING FOR A SECOND BABY
I am Dr Juliana Latif, the co-founder of Fusion Medical, which is a one-stop health screening practice located at Wheelock Place (Orchard).
I delivered my firstborn son at the age of 37 years old and put myself through 1 year of breastfeeding. The second month after stopping breastfeeding, my husband and I decided to continue with our family planning and scheduled our IVF procedure for our second child.
Little did I expect that my regular Breast Self Examination (BSE) done once a month would save my life. I detected a lump in my left breast when I was still breastfeeding my son. I thought it was just a blocked milk duct. Afterall, I was below the age of 40. An ultrasound check on this lump just a week before the scheduled IVF procedure turned my world upside down.
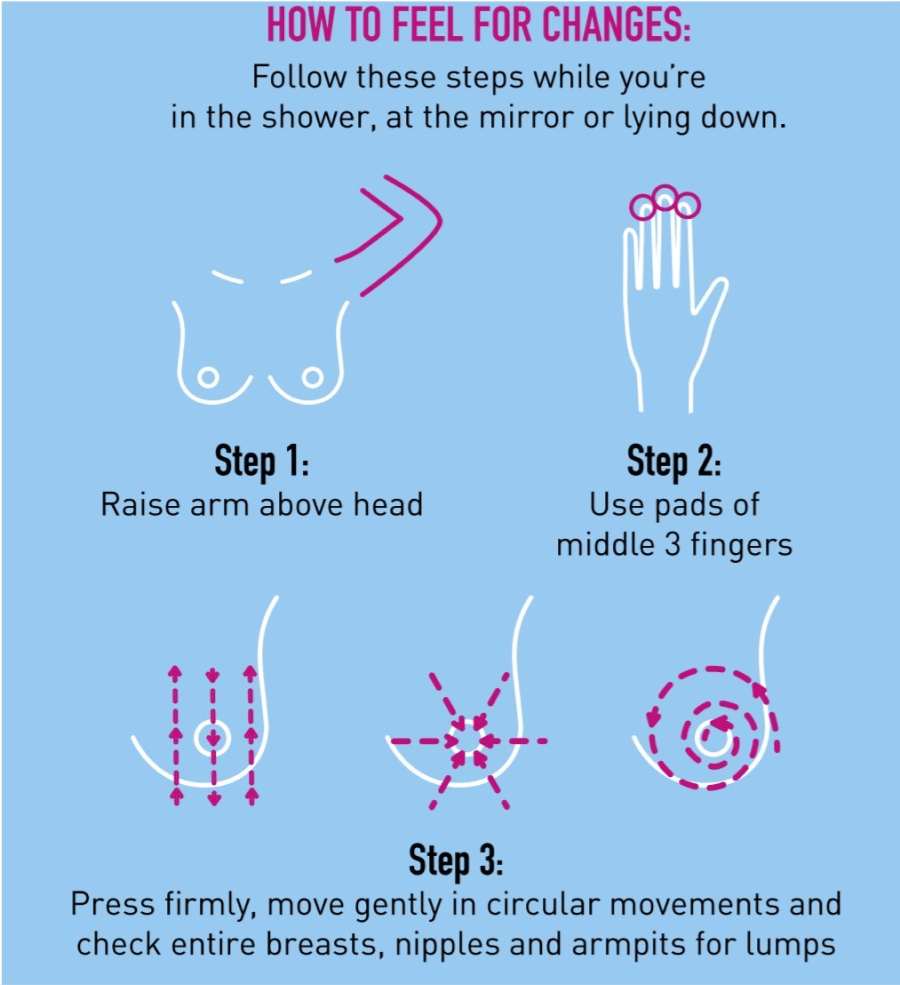
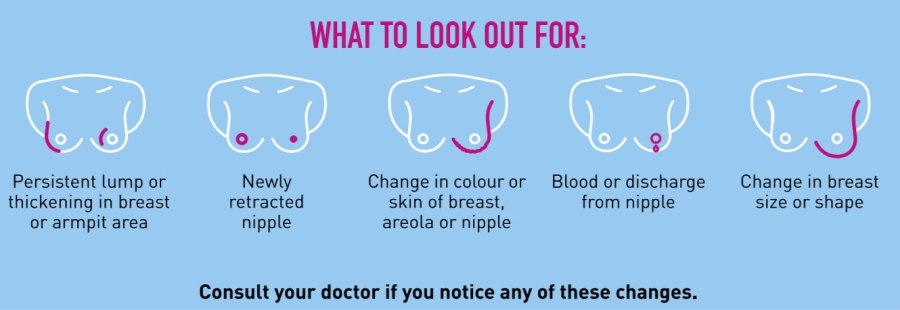
BREAST SELF EXAMINATION (BSE)
Because of my own personal experience, Fusion Medical has incorporated BSE in Fusion Deluxe Health Screening packages and above.
When should one start?
The Singapore Cancer Society recommends that women as young as age 20 can start doing monthly self-breast examinations.
BSE should be timed on a monthly basis 7-10 days from the start of your menstruation. If you have stopped menstruating, you can do your BSE on the same date each month.
*The images above were extracted from the Breast Cancer Foundation (Singapore). The full PDF file on breast self-examination can be found in the following link.
What happens when I detect a lump?
Additional checks would be advised upon discovery of a lump. These typically include breast ultrasound and /or mammography. You may wish to consider upgrading your mammography to that of a 3-dimensional one if you have a history of dense breasts.
Lumps that look suspicious on imaging will then require a biopsy to determine the nature of the cells. The good news is majority of breast biopsies do not turn out to be breast cancer. Follow up and treatment may still be recommended by the doctor to manage the benign lesion.
If cancer cells are found, a detailed report will be provided to determine the next steps in management. These include the tumour type and the tumour’s growth rate or grade.
What is important to note is to seek medical attention early. I was lucky that even though I ignored my breast lump initially, I was able to detect it early for the appropriate treatment to be administered. It was most heart-wrenching to kiss my one-year old son goodbye before tearing myself away from him for my PET/CT scan appointment to check if my cancer had spread. The two-hour long procedure was the longest journey of my life before I got informed that my cancer was localised.
Does discovery of a lump mean Breast Cancer?
My breast lump turned out to be invasive carcinoma.
However, you may be comforted and surprised to know that there are more benign (non-cancerous) breast conditions than cancerous ones:
a) Non-proliferative lesions: The most common being breast cysts and the increase in breast cancer risk is very small.
b) Proliferative lesions without atypia (cell abnormalities): These lesions have excessive growth or cells in the ducts or lobules of the breast but do not look very abnormal. They include ductal hyperplasia (without atypia), fibroadenoma and sclerosing adenosis.
c) Proliferative lesions with atypia: In these conditions, the cells in the ducts or lobules of the breast tissue grow excessively, and some of them no longer look normal. These types of lesions include ductal hyperplasia, atypical lobular hyperplasia and intraductal papillomas. Breast cancer risk is about 4 to 5 times higher than normal in women with these changes.
Nevertheless, despite the fact that these conditions are non-cancerous, having them can increase your risk of eventually developing Breast Cancer. Thus, it is important that you monitor these conditions on a regular basis, usually between 3 months to one year depending on what your doctor advises.
BREAST CANCER RISK FACTORS
Remember I talked about being young, thinking that this would not happen to me? Studies have shown that Breast Cancer is caused by a combination of risk factors and being young does not necessarily mean you will not get Breast Cancer. Risk factors increase your chance of getting a disease such as Breast Cancer, but having a risk factor doesn’t necessarily mean that you will get the disease:
Lifestyle-related Breast Cancer risk factors (this means that you can reduce your risk)
- Alcohol Intake
Alcohol has been clearly linked to an increased risk in Breast Cancer with the risk increasing depending on the amount of alcohol consumed. Having 1 alcoholic drink per day gives a small (7-10%) increase in risk compared with non drinkers, while having 2-3 drinks per day increases this risk to about 20% higher than non drinkers for developing Breast Cancer.
- Being overweight or obese after menopause
Before menopause a woman’s ovaries produces oestrogen for the body. After menopause fat cells take over this role, therefore women who are overweight after menopause will have more fat cells to produce more oestrogen thus increasing your risk of Breast Cancer.
- Physical inactivity
There is increasing evidence that proves that physical inactivity can increase Breast Cancer risk especially after menopause. According to the World Health Organisation (WHO) adults aged 18-64 should have at least 150 minutes of moderate-intense aerobic physical activity or at least 75 minutes of vigorous-intensity aerobic physical activity throughout the week.
- Reproductive history
Women who have their first pregnancy after the age of 30, or do not breastfeed have a slightly higher breast cancer risk overall. Having multiple pregnancies and becoming pregnant at an early age reduces Breast Cancer risk.
- Birth control
Oral contraceptive pills: Most studies have linked oral contraceptive users with a higher risk of breast cancer compared to non-users. However, this risk goes back to normal after 10 years.
Birth control injections: Depo-provera is an injectable form of progesterone that is administered every 3 months for birth control. Some studies have linked this type of birth control with an increased risk of Breast Cancer but some have not.
Birth control implants, Intrauterine devices (IUDs), skin patches, vaginal rings: As these types of birth control use hormones they could theoretically influence Breast Cancer growth. This link has been studied more in hormone-releasing IUDs but less on implants, patches and rings.
- Hormone Replacement Therapy (HRT)
There are 2 main types of HRT to control symptoms menopause in women: Combined HRT which have both oestrogen and progesterone and Estrogen-only therapy. The use of combined HRT after menopause has been linked to increased Breast Cancer risk. This risk is typically seen after 4 years of use with the risk decreasing after 5 years of stopping HRT. Regular monitoring during treatment should also be done.
Breast cancer risk factors that cannot be changed
- Getting Older
The risk of Breast Cancer increases with age; most new diagnosis of Breast Cancer occurs after age 50 but still significantly rises after age 40. Hence, the emphasis on getting a screening mammogram once you hit 40 years old. Our Singapore government has been very active in this area and do allow us to dip into our Medisave accounts or utilise their Screen for Life programmes.
- Genetic Mutations
About 5% to 10% of Breast Cancers are thought to be linked to hereditary gene changes (mutations) which are passed on from a parent. The most common cause for hereditary Breast Cancer is an inherited mutation in the BRCA1 or BRCA2 gene. (Think of Angelina Jolie here). Normally these genes are involved in repair of damaged DNA but mutated versions of these genes lead to abnormal cell growth, which can lead to Cancer.
On average, a woman (or man) with a BRCA1 or BRCA2 gene mutation:
a) has a 7 in 10 chance of getting Breast Cancer by age 80;
b) is more likely to be diagnosed with Breast Cancer at a younger age; and
c) has higher risk of developing Ovarian Cancer and certain other types of Cancers.
- Having a family history of Breast Cancer
Overall, about 15% of women with breast cancer have a family history of the disease. Having a first-degree relative (mother, sister or daughter) with Breast Cancer almost doubles a women’s risk. Having 2 first-degree relatives increases the risk further by about 3 folds.
- Age of menarche and menopause
Having early onset of menstrual periods before age 12 and menopause after age 55 expose women to hormones for longer, theoretically raising their risk of breast cancer.
- Having dense breasts
Breasts that are dense have more connective tissue then fatty tissue which can sometimes make it hard to see tumours on a mammogram. Women with dense breasts on mammogram had a 1 ½ to 2 times increased risk of breast cancer compared to a woman with average breast density.
SCREENING OF BREAST CANCER
Mammogram
A mammogram is a low dose X-ray picture of the breast. It can detect the presence of cancerous lumps even before they can be felt with the hand. Screening mammograms are routinely used to screen for breast cancer in women who have no specific symptoms. Diagnostic mammograms are done after a suspicious results, abnormal physical finding or screening mammogram. The diagnostic mammogram is to determine if these suspicious or abnormal findings are indicative of breast cancer. Compared to screening mammogram, diagnostic mammograms are more detailed .
What is digital breast tomosynthesis?
Digital breast tomosynthesis (DBT) is 3D mammography that allows the breast to be examined 1 layer at a time instead of 1 flat image. DBT may be used together with 2D digital mammography as an additional tool in screening. To the patient, the DBT experience is very similar to a 2D mammography and the X-ray dose remains very low and under the guidelines of FDA. To the radiologist who is the specialist reading the images, the DBT provides additional views of the breast to better analyse the breast tissue.
Ultrasound
A breast ultrasound is a scan that uses sound waves. The breast tissue deflects these waves causing echoes, which provide a picture of the breast tissue. It has the ability to differentiate between a mass that is filled with liquid from a solid mass. Ultrasounds are helpful when a lump is felt, and the images can be used to further evaluate the abnormality. It also helps to measure the exact size and location of the lump and analyse the surrounding tissue.
MRI
If initial diagnostic imaging is inconclusive, a breast MRI (magnetic resonance imaging) may be recommended. MRI uses magnetic energy and radio waves (not radiation) through the breast tissue to create a detailed picture which allows to distinguish between normal and diseased tissue.
Book your breast cancer screening now!
DIAGNOSIS IS THE START OF A LONG JOURNEY
I cannot overemphasise on the strong support that is required. My pillars of support would definitely be my husband first and foremost, followed by my mother, the rest of my family and the amazing support I got from my friends. My husband has walked beside me every single step of the way, giving me strength when I had none. He lovingly said to me: “I am with you always, the only place I cannot be with you is in your dreams”. Hence, when I was going through this dark period of nightmares and insomnia, I would wake him up and he would comfort me.
COVID-19 complicated my family’s situation as they resided in Malaysia and Brunei and were unable to fly in immediately to be with me during the initial diagnosis. We had to get special permission for them to fly in on compassionate reasons. COVID-19 strengthened my family bonds and I am so grateful that they endured the swabbing and quarantine on my behalf. I have always been very close to my family and having them with me was an integral part of my healing process.
I am also very thankful to my business partner Dr Wenus for shouldering the burden of managing the centre when I was away for about six months undergoing my treatment.
Being blessed with such strong support, I remained positive and was able to return back to a new version of my normal life. I hope through my experience I am able to help others by stressing on the importance of early detection and providing support for other cancer patients.
Vitamin D Deficiency
Vitamin D is an extremely important vitamin that has powerful effects on several systems throughout your body. It has a role in your nervous system, bones, muscle, and immune systems.
You can get vitamin D in three ways: through your skin, from your diet (eg oily fish, liver, egg) and from supplements. Your body forms vitamin D naturally after exposure to sunlight. But too much sun exposure can lead to skin aging and skin cancer, so many people try to get their vitamin D from other sources.
What causes Vitamin D Deficiency
Vitamin D deficiency is incredibly common and most people are unaware of it. That’s because the symptoms are often subtle and non-specific, meaning that it’s hard to know if they’re caused by low vitamin D levels or something else.
Vitamin D deficiency can be caused by the following reasons:
- Malabsorption or insufficient vitamin D in your diet
- Insufficient exposure to sunlight.
- Inability to convert vitamin D to its active form in the body.
- Medications that affect the body’s ability to convert or absorb vitamin D
Signs of Vitamin D Deficiency
1. Getting Sick Frequently
One of vitamin D’s most important roles is keeping your immune system strong so you’re able to fight off viruses and bacteria that cause illness. If you often become sick, especially with colds or the flu, low vitamin D levels may be a contributing factor.
2. Fatigue and Tiredness
Excessive fatigue and tiredness may be a sign of vitamin D deficiency. Taking supplements may help improve energy levels.
3. Depression
Low Vitamin D levels may impair cognitive function because there are vitamin D receptors in areas of the brain that are responsible for mood and behavior, including the development of depression.
4. Impaired wound healing
Vitamin D’s role in controlling inflammation and fighting infection is important for proper healing. Slow healing of wounds after surgery or injury may be a sign that your vitamin D levels are too low.
5. Bone or Back Pain and Loss of Bone Density
Vitamin D plays a crucial role in calcium absorption and bone metabolism. People with a deficiency are more likely to have weak bones, muscle weakness and back pain that limit their daily activities. Low bone mineral density is an indication that your bones have lost calcium and other minerals. This places older adults, especially women, at an increased risk of fractures.
6. Hair loss
One role vitamin D plays is stimulating new and old hair follicles. When there isn’t enough vitamin D in your system, new hair growth can be stunted.
Vitamin D helps to minimise risk of contracting COVID-19?
There have been reports of Vitamin D deficiency associated with higher risk of COVID-19. Medical Journal like JAMA Network Open also noted that patients with untreated Vitamin D deficiency were 1.77 times more likely to test positive for COVID-19. More studies are required before this conclusion can be reached.
Most will agree that there is no harm to add daily doses of vitamin D (400 to 1,000 units) in one’s supplement intake as it is generally safe. However, it is also possible that too much intake of vitamin D can cause toxicity and lead to an excess of calcium in the body which may not be desirable.
Do discuss with our doctor before starting on this vitamin regime.
S-Patch Cardio – 24 hrs Holter Monitoring
Leading Cause of Death
Worldwide, 27% of top 10 causes of deaths is related to cardiovascular disease (Heart Disease and Stroke). Arrhythmia is the major cause behind these causes of death.
According to statistics from the Singapore Heart Foundation, cardiovascular disease accounted for 29.3% of all deaths in 2019. This means that almost 1 out of 3 deaths in Singapore, is due to heart diseases or stroke. A study done by Singapore National Heart Centre and Health Sciences Authority in year 2003 estimated that as many as 1,000 died from Sudden Cardiac Death (unexpected death due to cardiac causes that occurs in a short time period in a person with known or unknown cardiac disease.” This condition is caused by an abnormal heart rhythm that disrupts the normal pumping of the heart throughout the body. There may be no warning signs or symptoms. About half of these deaths were less than 60 years old with 91% of them being males with the median age of 47 years old. For ladies, the median age was slightly higher at 50 years old.
What are abnormal heart rhythms?
Heart rhythm problems (heart arrhythmias) occur when the electrical impulses that coordinate your heartbeats don’t work properly, causing your heart to beat too fast, too slow or irregularly. Heart arrhythmias may feel like a fluttering or racing heart and may be harmless. However, some heart arrhythmias may be life-threatening.
Some people may not experience active symptoms due to arrhythmia. However, treatment is still essential for preventing further complications, which may include stroke and heart failure.
Symptoms of heart arrhythmias include:
- Palpitations (Missed beats, Skipped beats, Fluttering in the chest)
- Racing or slow heart rate
- Lightheadedness or dizziness
- Fainting or near fainting
- Chest pain
- Shortness of breath
What increases the risk for an arrhythmia?
- Personal or family history of coronary heart disease, other heart problems, high blood pressure, diabetes
- Increasing Age
- Obstructive Sleep Apnoea
- Electrolyte Imbalance (eg potassium, sodium, calcium and magnesium) can trigger and affect the heart’s electrical impulses and lead to arrhythmia
- Chemical agents or substances such as caffeine, alcohol, tobacco and certain medications
How are arrhythmias diagnosed?
Traditional screening tests like stress treadmill and 12 lead ECG captures a snapshot of the heart function at the point in time. The following tests offer monitoring over a longer period of time, and therefore provide a more accurate diagnosis of arrhythmia.
Holter monitor. A Holter monitor is a continuous ECG recording done over a period of 24 hour or more. Traditional holter monitors have electrodes that are attached to your chest and connected to a small portable ECG recorder by lead wires. Holter monitoring may be done when your physician thinks you may have an arrhythmia.
S-Patch Cardio offers an alternative ECG Monitoring of up to 72 hours that may be more user-friendly and cost effective. It involves a small electrocardiogram monitoring device that weighs 11 grams versus traditional holter monitors which are bulkier and heavier at 800 grams. Data is automatically transmitted to the cloud for easy retrieval by authorised parties. Results are validated by cardiologists although the equipment is being dispensed by a General Practitioner.
As there may be no symptoms, early detection may be your best option. Discuss your concerns with our doctors today.